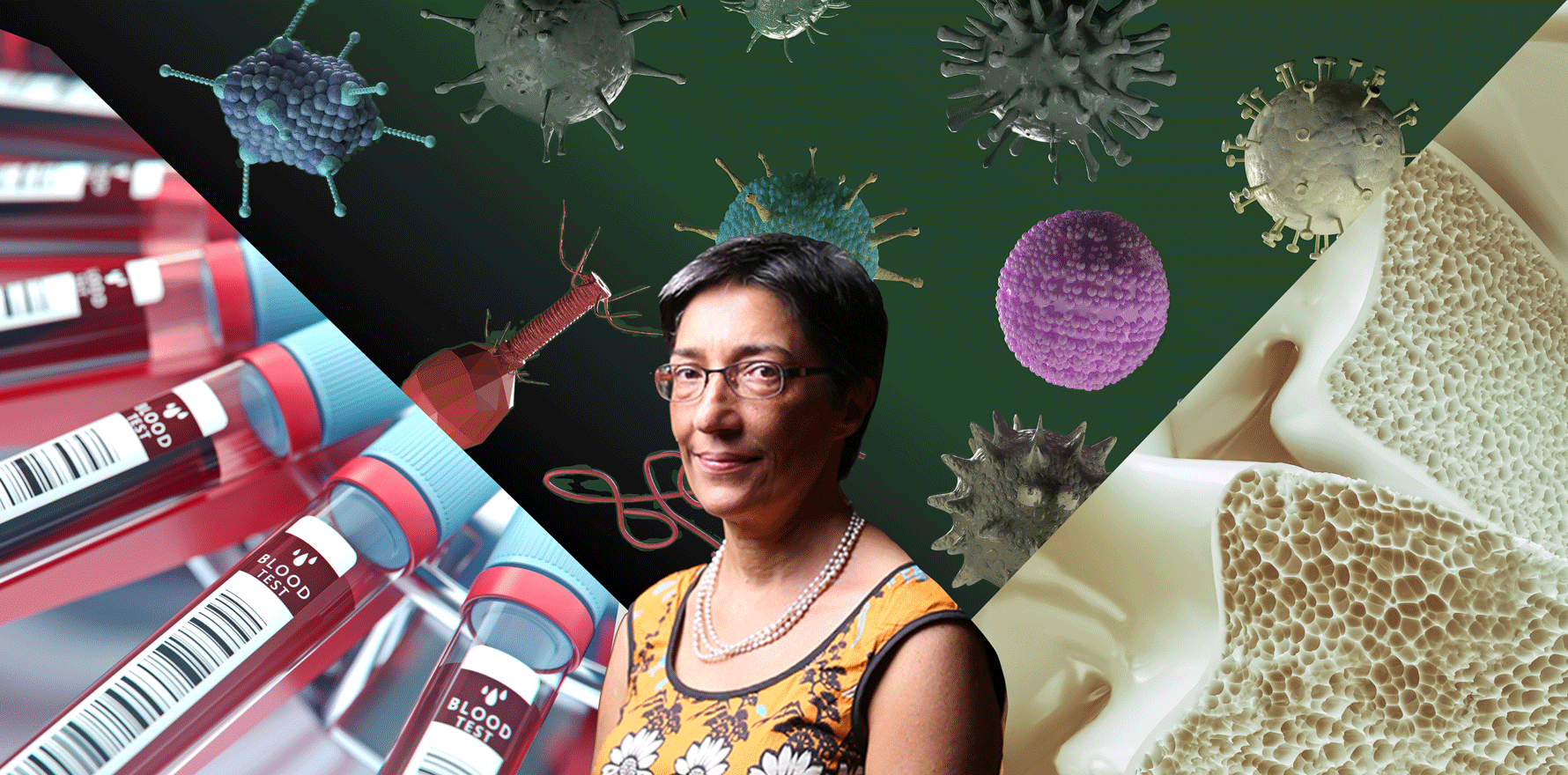
Professor Ranjeny Thomas takes us through her selection of the best rheumatoid arthritis presentations from ACR 2022.
We asked four leading Australian rheumatologists to talk us through research presented at ACR 2022 that will change practice now and in the near future, as well as research that excites them.
In this article we feature rheumatoid arthritis research as selected by Professor Ranjeny Thomas.
For the research that will change practice now, Professor Thomas chose the late breaking abstract L01 Impact of glucocorticoid dosing and anti-osteoporotic treatment on bone health in patients with inflammatory rheumatic musculoskeletal diseases: A longitudinal cohort study.
The Italian study included 884 women with inflammatory rheumatic musculoskeletal diseases treated with glucocorticoids and followed them for up to six years. Bone mass density (BMD) was significantly decreased in patients not taking anti-osteoporosis treatment at all GC doses. However, BMD remained the same or even increased in those taking less than 5mg/day GC per day plus anti-osteoporosis treatment (there was still a decrease in those taking 5mg or more).
The incidence of fragility fractures was higher among the RMD cohort than disease-free matched controls, with those taking 5mg/day or more at two-fold greater risk compared with all other doses.
“My takeaway from this is that fragility fracture is a preventable harm arising from low dose glucocorticoids, and it’s surprising just how low that dose can be to lead to harm over a period of years,” said Professor Thomas.
“So think about doing a baseline bone mineral densitometry. And remember that when you’re starting steroids, it may be difficult to get people off. So while you might think that you’re starting for a short period, that may balloon out to years – and there’s an increased risk of fracture as those years wear on, even at very low doses.
“Monitor the steroid duration, and be proactive with follow-up bone mineral densitometry, with intervention if it’s warranted.”
Next in Professor Thomas’s selection was The Great Debate: To treat or not with DMARDs in subclinical rheumatoid arthritis.
“The background to this is that subclinical RA – which includes positive auto antibodies, or rheumatoid factor, and all subclinical synovitis – that precedes clinical arthritis is an increasingly common scenario in rheumatology practice, but it’s unclear how to manage these patients,” said Professor Thomas.
Broadly, the ‘for treatment’ team argued that once someone has RA, they have it for life, so prevention is better than cure.
However, prevention is far from assured. There have been some positive findings, such as the ARIAA abatacept study (abstract 0530) which reported delayed RA onset for 18 months and VITAL, which found omega 3 and vitamin D supplements reduced risk of incident autoimmune disease. But abstract 1604 showed no effect with hydroxychloroquine in ACPA+ patients with clinically suspect arthralgia.
The ‘against treatment’ team argued that most preclinical cases do not go on to develop RA – perhaps only one out of six do. So many patients would be unnecessarily treated, suffering medication side effects and creating additional burden on the health system.
“The bottom line is that neither team actually believed that we should be treating pre-RA with DMARDs in 2022, said Professor Thomas.
“I chose this because it will be an intense area of research, drug development and trials. And to reiterate that recruiting an Australian cohort of pre-RA is very important to understand what our local risks are, to develop biomarkers and participate in trials including lifestyle interventions.”
For the research that excited her most, Professor Thomas chose 0535 Increased Rates of Bacterial Infection in Patients with ‘Pre-RA’.
The Scottish study found that infections were more common in patients with pre-RA and RA than in age/sex/neighbourhood matched controls. The risk rises more one year prior to the diagnosis of RA and treatment with methotrexate, and then remains stable in the first two years of the disease.
As to why, it could be that infection may hasten the progression through the pre-RA phases, or alternatively, disease-associated immune dysfunction in pre-RA may predispose to infection.
“The other thing that they discussed was bidirectional or positive feedback,” said Professor Thomas.
“And what might be happening is that there’s infections promoting progression of autoimmunity to rheumatoid arthritis. We could hypothesise here that it involves inflamm-ageing of T and B cell repertoire, with a progressive reduction in reserve so that as you get one infection, and then another infection, there’s fewer and fewer naive T cells and B cells in the repertoire that can cope with those infections.
“And then we know that infection promotes NET formation in neutrophils, and that they can bind to ACPA and that potentially could lead to more pro-inflammatory progression of the disease.
“So I think that the bidirection was a really very interesting possibility.”
Ranjeny Thomas is a professor of rheumatology at University of Queensland Diamantina Institute, and a rheumatologist at Princess Alexandra Hospital. In 2020 she was recognised for her outstanding contribution to medical education and research when she was awarded Member of the Order of Australia.
Rheumatology Republic invited Professor Ranjeny Thomas, Associate Professor Alberta Hoi, Associate Professor Peter Wong and Professor Peter Nash to present three of their favourite ACR 2022 abstracts in a webinar held at the conclusion of the conference. We’ll feature the research highlighted by each guest over the coming weeks.
In the meantime, you can see a recording of the full webinar here.