Respiratory bugs could trigger systemic autoimmune rheumatic disease, research suggests.
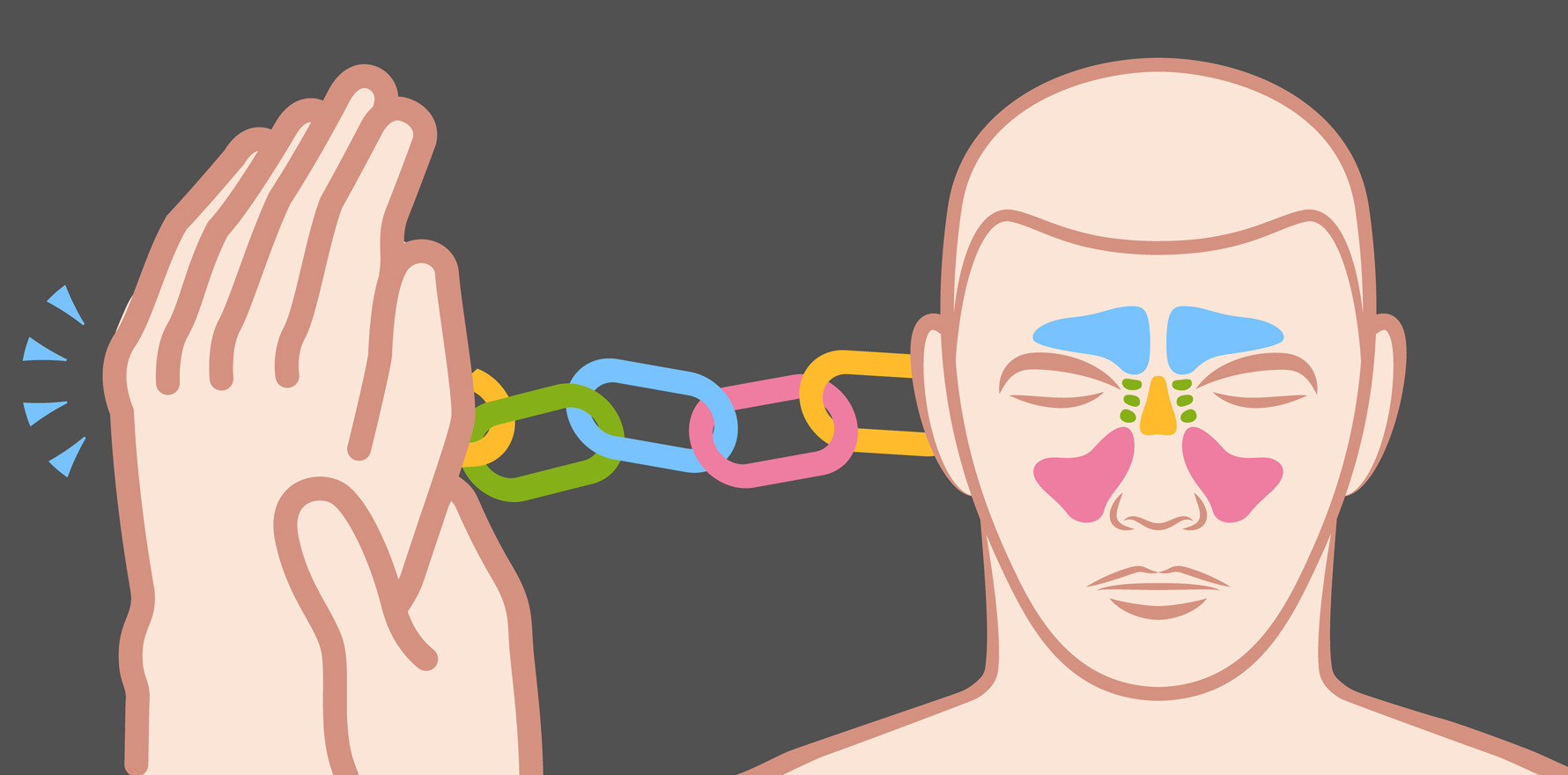
Mayo Clinic researchers have linked a history of sinusitis with a 40% increased risk of rheumatic disease.
This suggests sinusitis may play a role in the pathogenesis of rheumatic diseases and could therefore be a potential target for prevention and/or treatment, said researchers led by rheumatologist Dr Vanessa Kronzer.
“In this population-based cohort of incident rheumatic disease cases and controls, preceding sinusitis was associated with increased risk of multiple incident rheumatic diseases, especially antiphospholipid syndrome and Sjögren’s disease,” wrote the study authors in RMD Open.
“In general, the association between sinusitis and rheumatic diseases was strongest in the 5–10 years before disease onset and increased in a dose-response fashion with the number of sinusitis codes,” they wrote.
“Finally, the association between sinusitis and rheumatic disease was stronger among never smokers. These findings provide novel insights related to the pathogenesis of rheumatic diseases.”
Using a medical record database covering people living in Minnesota, the researchers identified over 1700 cases of rheumatic disease diagnosed between 1995 and 2014, with each case matched to three controls.
They looked for a history of acute or chronic sinusitis recorded at least one year before the rheumatic disease diagnosis.
Overall, precedent sinusitis was associated with a 40% increased risk of rheumatic diseases, though for some there was greater risk than others.
Antiphospholipid syndrome had a seven-fold increased risk and Sjögren’s syndrome more than double the risk, while vasculitis and polymyalgia rheumatica had a 40% greater risk. For seronegative rheumatoid arthritis there was an 80% increased risk.
The association was strongest where sinusitis occurred in the 5-10 years before disease onset, which the authors say argues against reverse causation. There was also a dose-response effect – the greater the number of sinusitis episodes, the higher the risk of rheumatic disease.
The authors cautioned that the findings may not be generalisable to all populations, as the study population was mostly white and rheumatic disease outcomes vary by race and ethnicity. Also, patients are more likely to seek medical care for more severe sinusitis, so the findings may not apply to all severities of sinusitis.
The link between rheumatic diseases and respiratory irritation, caused by smoking, silica exposure, air pollution, occupational inhalation exposure and respiratory tract diseases, is well documented. An association between sinusitis and RA and ANCA-associated vasculitis has also been reported. However, the authors said, prior to this study, a potential link between sinusitis and other rheumatic diseases hadn’t been investigated.
The authors suggested that one potential explanation “could be that pathogenic organisms such as those involved in sinusitis play a causal role in disease. Indeed, both Staphylococcus and more recently Corynebacterium were implicated in pathogenesis of ANCA-associated vasculitis whereas Ruminococcus gnavus was associated with lupus nephritis, RA and spondyloarthritis”.
“Furthermore, sinusitis is associated with accelerated atherosclerosis, further supporting its potential inflammatory effects,” they wrote.
“Therefore, future studies should replicate the observed association between sinusitis and rheumatic diseases, search for additional causative organisms and determine whether preventing or treating sinusitis can prevent and/or treat rheumatic diseases.”