The current supply of trainees risks not meeting future needs, rheumatology workforce survey finds.
One of the most keenly anticipated sessions at the ARA ASM was the results of the 2021 rheumatology workforce survey.
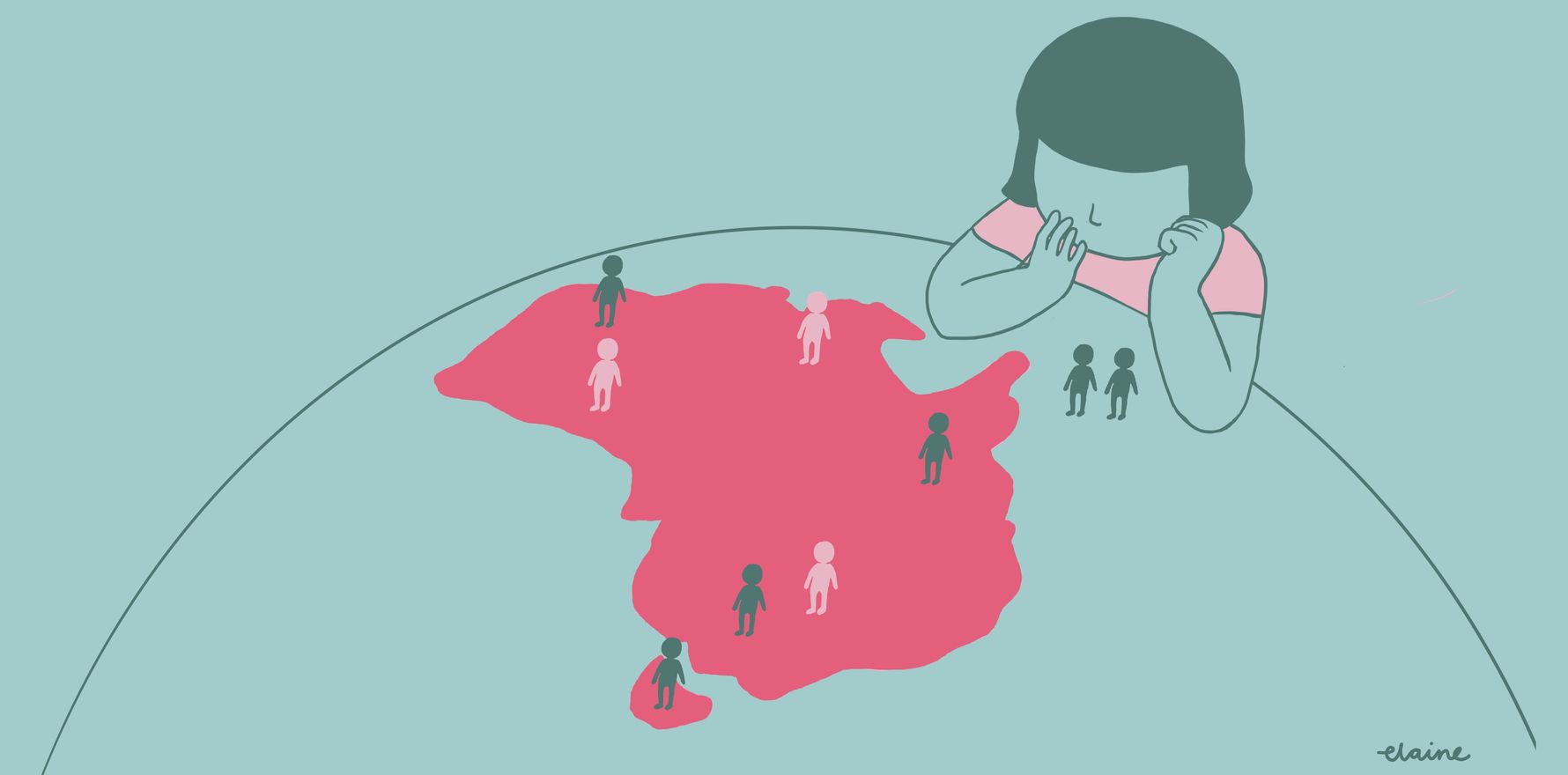
Presented by Professor Catherine Hill, the findings showed that Australia had an under-supply of both adult and paediatric rheumatologists, especially in regional and rural areas – and with projected decreased working hours over the next two years, it’s set to get worse.
In raw numbers, there were 380 adult rheumatologists, a number that fell slightly short of the 400 rheumatologists needed to fulfil the estimated ideal number, based on two rheumatologists per 100,000 adults.
However, most survey respondents indicated they were not doing a full-time clinical rheumatology load, with a median of six half-days per week. Based on reported clinical workload, therefore, current numbers equated to 231 full-time-equivalent positions – well short of the 400 needed.
This situation was even worse for paediatric rheumatology, as was raised at the recent parliamentary inquiry. There were 25 paediatric rheumatologists working a clinical full-time-equivalent of 13, which again was well short of the ideal of 32 (based on one per 200,000 children).
Based on current workloads, the estimated shortfall in rheumatologists was 278 adult and 36 paediatric rheumatologists.

The survey also found that while 10% of rheumatologists were considering increasing their work hours, 38% were considering reducing their workload temporarily or permanently, mostly within the next two years.
The survey analysis considered several trainee scenarios over the next 15 years. If current levels were maintained – that is, around 17 to 18 finishing per year – the ideal number of rheumatologists might be met by 2038. However, that number was based on a rheumatologist count, not the actual clinical hours worked – and if workloads continued at their current level, the ideal number would never be met unless trainee numbers were almost doubled.
“Now, this doesn’t take into account the ageing of our population, or the possibility for an increased demand for our services – for example, if there was a change in therapeutics that required extra input by rheumatologists,” said Professor Hill.
The situation for rural and regional rheumatology was particularly problematic, with only about a quarter of rheumatologists doing regional and rural clinics, typically one clinic per month. These were more likely to be older rheumatologists than younger ones, and males more than females. No paediatric rheumatologists reported doing rural or regional clinics.
The good news was that work satisfaction was high, with 80% satisfied or very satisfied with their work.
“It’s a bit less of females,” Professor Hill pointed out, “but overall, we have very good job satisfaction.

Work-life balance was reasonable, with almost half extremely or very satisfied with work-life balance, with males more satisfied than females, and the youngest and oldest cohorts more satisfied than those in the middle years, especially 45-64, when people were working more.
As for the future, the ARA would advocate for increased advanced training positions. As Professor Hill said in wrapping up the session: “At the current rate, we’re never going to meet ideal numbers, in our lives, in the lifetime of my career and in many other careers. I think it really shows that we need probably at least 75% to 100% more trainees to meet the demand”.
The lead image was provided by Dr Elaine Ng, a rheumatology advanced trainee who enjoys drawing.