A big Australian study adds more about the limitations of vitamin D supplements.
A large Australian population-based trial of monthly vitamin D supplementation has failed to show any benefit in reducing fractures.
The D-Health trial was led by Professor Rachel Neale, a cancer researcher at the QIMR Berghofer Medical Research Institute in Brisbane, and was published in The Lancet Diabetes and Endocrinology.
Over 21,000 people aged 60-84 were recruited from the electoral roll for the study, with participants from all six states and the ACT. People taking more than 500 IU of supplemental vitamin D and those with a history of osteomalacia, among other conditions, were ineligible to take part. Baseline serum 25(OH)D was not tested.
Participants were randomised 1:1 to receive a monthly 60,000 IU dose of vitamin D3 or placebo for just over five years. They completed a survey annually to collect information on adherence, and 800 people were randomly selected each year for a blood sample.
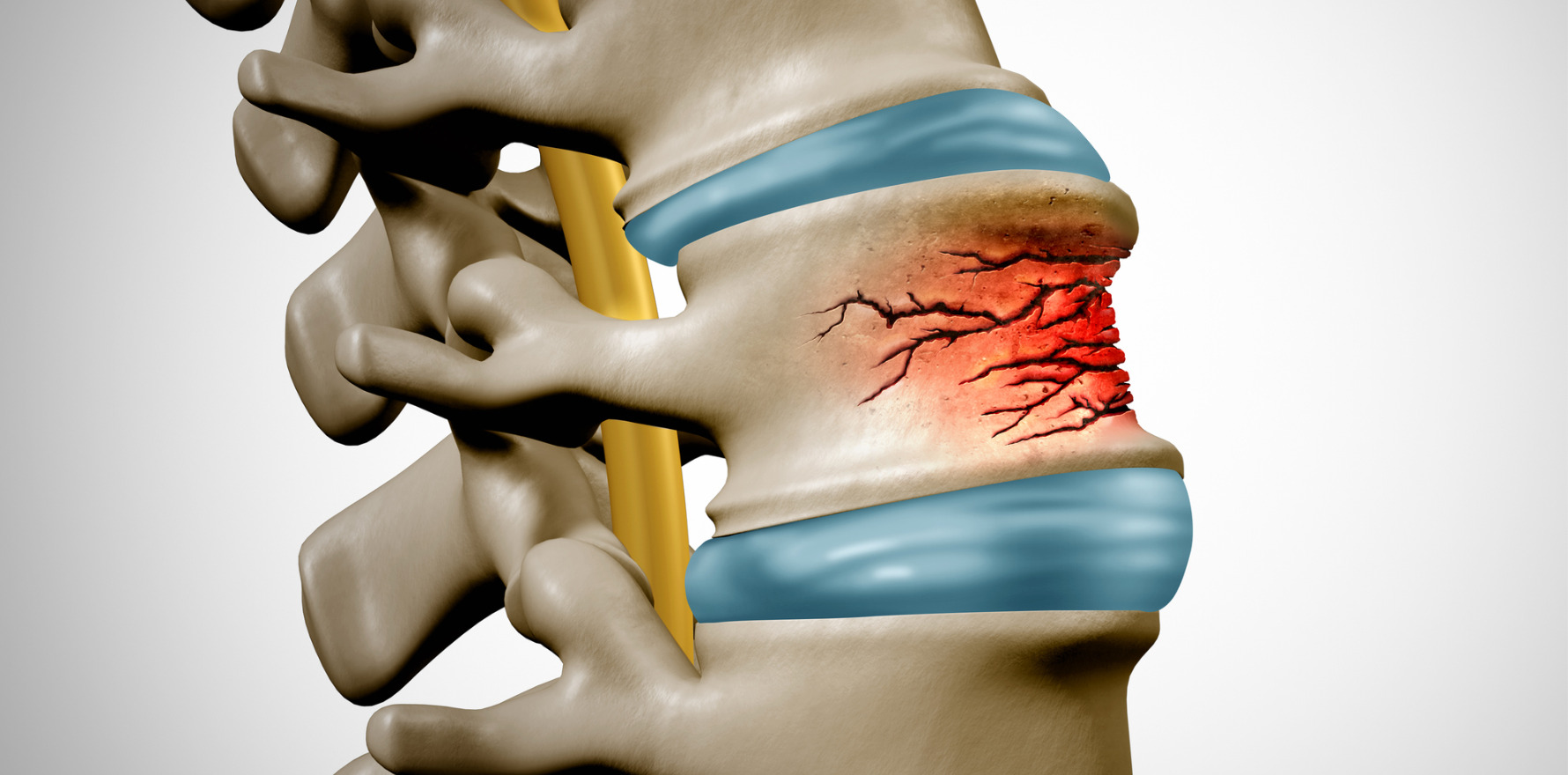
The main outcome for this analysis of the D-Health data was total fractures, with information obtained from hospital admissions and the national MBS database. Additional outcomes were non-vertebral fractures, major osteoporotic fractures and hip fractures. Repeat fractures weren’t considered and participants were censored after the first fracture.
Over the trial period, 5.6% of the vitamin D group and 5.9% of the placebo group had at least one fracture, a non-significant difference.
There was no interaction with time (p=0.14) but there was a difference at the five-year mark (HR 0.83, 95% CI 0.69-0.99). The number needed to treat to prevent one fracture was 303. For the fracture subgroups, there were no significant differences.
Among men, who made up around 54% of the study population, there was a slight, but non-significant benefit of vitamin D supplementation (HR 0.85, 95% CI 0.71-1.01). This became more pronounced as time progressed, and the difference at five years was significant (HR 0.71, 95% CI 0.55-0.93).
As noted earlier, the baseline 25(OH)D levels were not measured. However, based on sampling that occurred throughout the trial, it was estimated to be about 77nmol/L, with only about 13% of participants likely to be deficient (<50nmol/L). As such, the study results can’t be extrapolated to those with vitamin D deficiency.
There were several factors associated with increased rate of fracture, including advancing age, female sex, being treated for osteoporosis, poorer quality of life, declining overall health, BMI less than 25 and predicted baseline 25(OH)D concentration 50nmol/L or less.
“Overall, we did not find an effect of monthly doses of 60 000 IU of vitamin D3 on fractures,” concluded the authors.
“However, there was some evidence for a trend consistent with benefit after a follow-up period of 3·5 years. Vitamin D supplementation did not appear to reduce the overall incidence of nonvertebral, major osteoporotic, or hip fractures.”
A positive outcome was the finding that taking the vitamin D in a monthly bolus – a convenient regimen for many patients – did not appear to increase the risk of falls, contrary to findings from other trials.
The strengths of the study were the very large general population cohort and the long treatment duration. Limitations include the lack of baseline serum 25(OH)D measures and the lack of applicability to populations with a higher prevalence of vitamin D deficiency.
In a linked comment, Professor Ian Reid a prominent bone research expert from the University of Auckland, noted that “the D-Health study’s primary findings agree with those of the large trials and the previous meta-analyses, that vitamin D supplementation in vitamin D-replete, community-dwelling cohorts does not have an effect on fracture risk, or on any other major clinical endpoint”.
As for the apparent benefit noted in the later stage of trial, he suggested that could be a statistical anomaly, with the drop in numbers towards the end perhaps contributing to the difference.
“The abrupt appearance of a treatment benefit in the last year of a five-year study is unprecedented in fracture-prevention trials with any agent,” Professor Reid pointed out.
While acknowledging the value of the finding that taking a convenient monthly bolus was safe, Professor Reid suggested that based on the overall findings of this study and similar studies, such as the five-year VITAL study, “further trials of vitamin D on skeletal endpoints in vitamin D-replete populations are not justified”.
However, he concluded, “The effect of vitamin D on non-bone endpoints (e.g. diabetes, cardiovascular disease, and cancer) in severe vitamin D deficiency (25-hydroxyvitamin D <30 nmol/L) remains uncertain, and might justify the need for new trials; although, it could be argued that intervention is already justified to prevent osteomalacia in these populations.”