Cumulative doses over long periods aren’t associated with higher fracture risk, with or without osteoporosis.
While prolonged systemic steroid use is associated with higher fracture risk, injected corticosteroids in clinical practice are not, even for patients with osteoporosis, according to a US study published in JAMA.
“We hypothesized that higher fracture risk would be associated with increasing cumulative injected triamcinolone equivalent doses,” the authors wrote.
But the study, conducted at the Mayo Clinic in Minnesota, found that it wasn’t.
The single site cohort study included more than 7000 people, 62% women and 93% white, who received any corticosteroid injection (methylprednisolone, triamcinolone, betamethasone, or dexamethasone) from the beginning of May 2018 to the end of June 2022.
Fewer than one in 10 had inflammatory arthritis (8.2%). Nearly nine in 10 participants had either osteoarthritis or bursitis. Of these, 6% had at least one episode of acute crystalline arthritis (gout or pseudogout) during the study, 7% had an episode of acute joint pain from conditions such as knee meniscus tear or shoulder adhesive capsuliti, and 0.4% had hemarthrosis.
Of those without osteoarthritis, 4% crystalline arthritis, 7% had a diagnosis of knee meniscus tear or shoulder adhesive capsulitis and 0.2% had hemarthrosis.
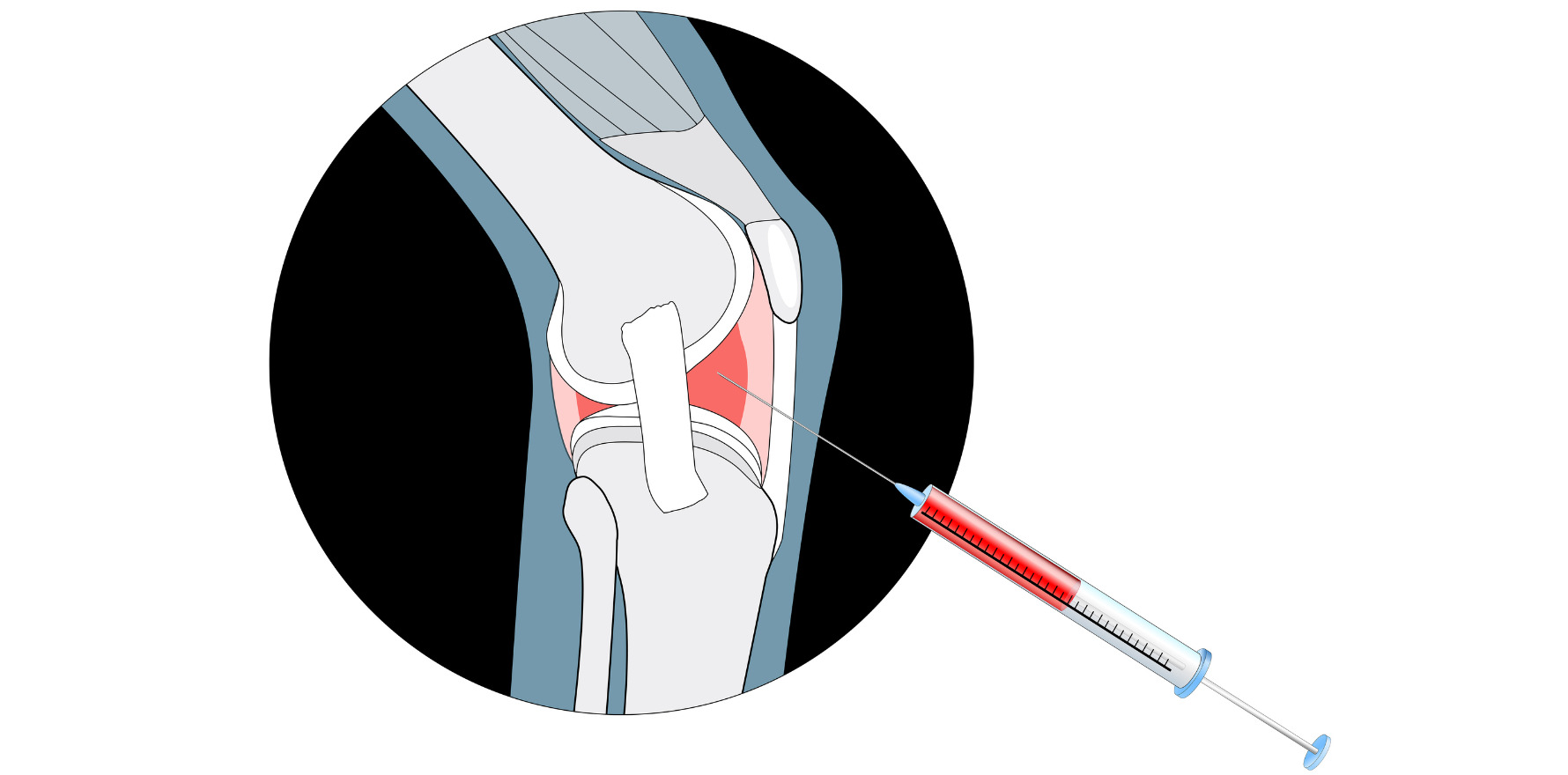
The mean total cumulative injected corticosteroid dose received during the study per person was 141.8mg of triamcinolone equivalent. Most injections (45%) were received in large joints, with the next most common site being the spine facet (19%).
During the study, 5% (346) of the patients at the Mayo Clinic in Minnesota USA suffered a fracture, 43% of which were considered osteoporotic. Only 2% of the fractures were in the non-high-risk group, with 23% of those considered osteoporotic.
The only factors that were associated with higher fracture risk were age, Charleson comorbidity index, and previous fracture.
It’s not particularly surprising that corticosteroid injections didn’t lead to fractures in a group of people with osteoarthritis, said rheumatologist Professor David Hunter, chair of the Institute of Bone and Joint Research at the University of Sydney.
“There’s an inverse relationship between the incidence of osteoporosis and osteoarthritis. So as a consequence of them having less osteoporosis, they’re less likely to fracture, irrespective,” said Professor Hunter.
The researchers said “clinicians should be reassured that frequent CSI is not associated with higher fracture risk and should not withhold these important pain treatments owing to concern for fracture”.
But Professor Hunter saidsystemic harm was not something that is normally a concern with injected corticosteroids, unlike with oral corticosteroids, because they are administered intermittently and infrequently.
“Generally, in clinical practice, we’d say you don’t want to inject a joint more frequently than once every three to four months. And most people may just have a one-off injection,” he said. Injections come with other risks, like discomfort, infection and skin breakages. Furthermore, the drugs leave the system within 48 hours, making the chance of systemic toxicity “negligible”, he said.
“Prolonged, systemic steroid use is associated with risk of fracture. I would be incredibly surprised if the doses and the duration of exposure from injections were sufficient to cause any concern,” he said.