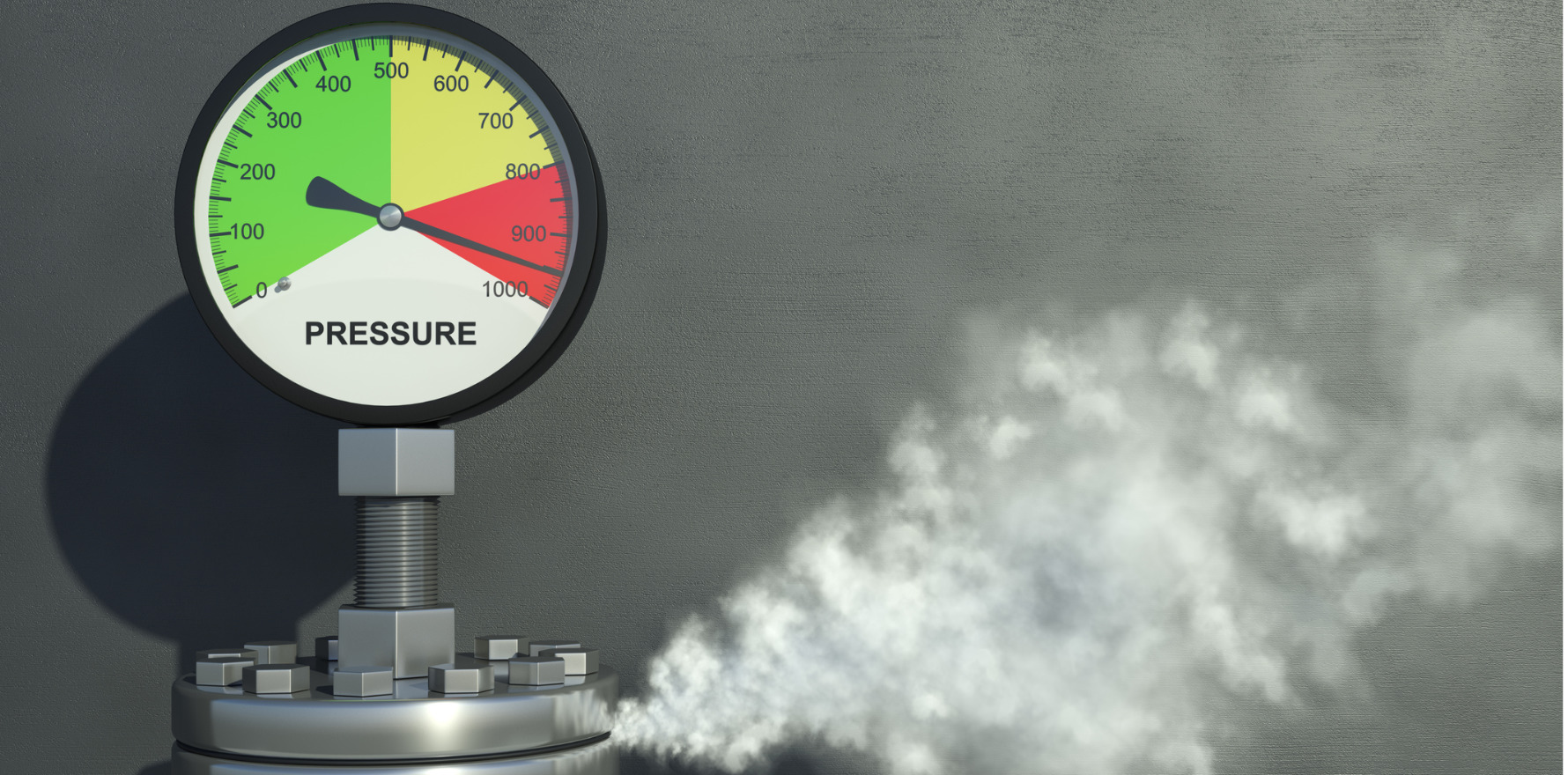
OPINION | Try writing some guidelines for everyone, in every situation, under intense scrutiny, with no direct evidence, that fits into all governance structures, and do it yesterday, s'il vous plaît.
Well, it was always going to come to this – COVID vaccine talk is everywhere you look.
If you happen to have read Jeremy Knibbs’s editorial for The Medical Republic a few weeks ago, you’ll know Australia needs to hit a furious pace of 200,000 vaccinations/day to make the self-imposed October deadline (which the economy is hanging on), and every day we fall behind the required run rate goes up. The hustle is justified, but just as the dust was settling from 2020 and we were entering some form of normal, we now have to spring back into the best of pandemic traditions: uncertainty and rapid decision making.
Some of you might know that apart from being a rheumatologist I’m also a clinical pharmacologist, and in that role I’ve been involved with the vaccine (well, my team’s done the heavy lifting) – in particular, designing a scalable implementation plan for vaccine cold chain and reconstitution for use by hospitals around the country for the Pfizer-BioNTech vaccine and its fickle -70°C multi-dose vial current needs.
It’s been far more complex than I ever realised. While it seemed achievable enough at the beginning, it’s challenging to design something:
(a) that everyone in diverse situations can use on aggressive scale, but with sufficient detail to actually be useful
(b) in a high-scrutiny, high-complexity space, extrapolating the limited available information with only ill-fitting precedents
(c) that fits into the demands of multiple layers of governance, each of which is understandably concerned about the domains they’re responsible for, but none of which have the capacity to provide the detail to make it happen
(d) happens far too quickly.
So it’s probably predictable that I feel a little bit sympathetic to the plight of guideline writers in the rheumatic disease COVID-19 vaccine space.
In the next few months, all of our patients will be offered the vaccine, and almost all of them who accept it will care about meaningful protection. How do we optimise this, while keeping our patients’ disease under control, our patients away from confusion and belief in the vaccine high without calling every patient to tell them what to do? It’s essentially impossible to get right.
Try writing some guidelines for everyone, in every situation, under intense scrutiny, with no direct evidence, that fits into all governance structures, and do it yesterday, s’il vous plaît.
We’ve recently seen the first version of the ACR guidance released, on the background of BSR and ARA guidance, and it evoked a few grumblings which were perhaps inevitable. While no-one really questioned the rituximab guidance, the questions flew quickly: why pick on methotrexate and why one week, why the trickery around abatacept for the first vaccine dose and not the second, why shouldn’t we test for antibody response to know if it’s worked, and how would any of this work in practice anyway?
Well, to its credit, the ACR came out and talked through its guidance, and really explained the process (as rigorous as practicably possible) and the thinking (which helped some things make sense). More than that though, a few points about this situation are worth considering:
- I don’t actually know best. I am not a rheumatic disease vaccine specialist; I don’t have the sophistication of one, I don’t have the balance of a group of them in a consensus building exercise, and I definitely don’t have the time to go through all the data. If I can option out some of the thinking on this to smart people who are specifically much smarter about these things than I am, and get their considered advice, I’ll always take that over my corridor guesswork.
- What are guidelines anyway? It’s not meant to be a cookbook, and I never follow the recipes exactly anyway (more salt, more garlic, I try to skimp on the butter but it never tastes as good). It’s not meant to be a legal demand; the documents make that clear. They’re just general suggestions to try and drape across the elaborate topography of our patients’ clinical situations.
- These are ‘living guidelines’, based on what we know in a rapidly moving space. We need something now, we need to tell our patients something very soon, and to have a structured process where that’s updated as things happen is a genuine blessing.
- Don’t we agree on the most important things anyway – that our patients should definitely get vaccinated? Who said we’ve got nothing in common?
- If things aren’t exactly how we think they should be, how should we feel about that? The COVID era necessitates a certain level of generosity of spirit; isn’t this the time for it?
Personally, and this is just my opinion: I think we should cut the authors some slack and just be a little bit grateful for putting in the hard yards and getting something out. And maybe even thank them.
As Wesley Snipes said in that early 1990s bedrock American movie, New Jack City: I wouldn’t wanna be ya.
Different opinion? Let us know in the comments or by writing to david@medicalrepublic.com.au