Buprenorphine as a patient’s first opioid doubles the odds of persistent use compared to other drugs in the class.
Think low and steady, not slow(-acting) and steady.
Opioid use remains high despite disagreement over their potential benefits and the growing awareness of the increased risks of adverse outcomes that accompany their long-term usage. Numerous policies have been designed with the aim of minimising the amount of people who become persistent opioid users, but specific risk factors of who is at risk of persistent use are not clear.
A new Australian study, published in Pain Medicine, provides some insight into the predictors of persistent opioid use, reporting that the initially prescribed opioid can double – or more than halve – the odds of becoming a persistent user.
“Some of the strongest predictors of persistent opioid use were opioid prescribing practices, such as prescribing high opioid quantities, providing repeat prescriptions and prescribing long-acting opioids at [the] commencement of opioid therapy,” the researchers wrote.
“These factors may help identify people at risk of persistent opioid use and enable opportunities to implement early intervention and additional pain management strategies for these people.”
As part of the retrospective cohort study, researchers examined electronic health and prescribing data for 340,000 patients who initiated opioid therapy for non-cancer pain in 560 general practices across eastern Victoria. Seventeen percent of patients had been diagnosed with a musculoskeletal condition in the 12 months prior to initiating opioid therapy.
Included patients had not been prescribed opioids in the 12 months prior to the start of the study. Patients prescribed opioid replacement therapy in the year before the study were excluded.
Persistent opioid use (defined as being prescribed opioids more than 90 days after the patient received their first opioid prescription with a gap of less than 60 days between subsequent prescriptions) occurred in 4.8% of patients.
After accounting for factors such as age, sex, socioeconomic status, comorbidities, opioid characteristics and whether the patients were prescribed other medications, patients, patients initially prescribed buprenorphine had 1.95 times the odds of developing persistent opioid use compared to patients who were prescribed a different opioid initially.
In contrast, patients prescribed oxycodone in the first instance had 0.89 times the odds of developing persistent opioid use compared to patients not prescribed oxycodone in the first instance, while patients initiated on codeine had 0.26 times the odds of developing persistent opioid use compared to patients who did not receive codeine.
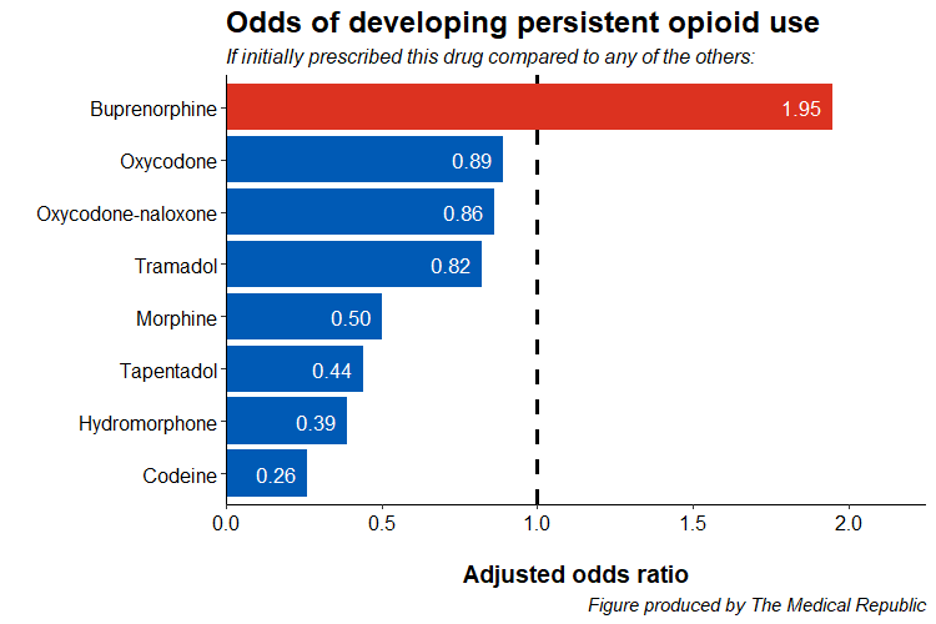
Researchers felt the increase in odds seen in patients receiving buprenorphine and the decrease in odds in patients receiving codeine were due to their respective indications for severe/persistent pain and mild pain, which could potentially indicate the level of pain reported by the patient.
“It’s also possible to speculate whether the longer duration of buprenorphine may be associated with greater persistence,” the researchers wrote.
Receiving a prescription for a long-acting opioid straight off the bat was associated with 2.07 times the odds of developing persistent opioid use compared to patients prescribed short-acting opioids, and a patient give repeats with the initial prescription had 2.94 times the odds of developing persistent opioid use.
Increasing age, female sex and the presence of comorbidities such as depression or anxiety, sleep disturbances and substance use disorder were among the other factors also associated with increased odds of developing persistent opioid use.
Codeine combinations (e.g., paracetamol/codeine) were the most commonly prescribed initial opioid therapy (60.9% of patients), ahead of oxycodone (12.2%), single ingredient codeine (8.7%), tramadol (8.6%), buprenorphine (1.9%) and morphine (1.2%).
The findings of the study are limited by the researchers only looking at prescribing, rather than dispensing and/or usage data, and the fact that the indication for the initial opioid prescription was unknown.
Between 2013 and 2017 almost two million Australians started using opioids each year. In 2017 over 50% of unintended deaths were opioid-related, while 56% of opioid related-deaths involved prescription opioids.




