A 51-year-old male patient had been experiencing progressively worsening right hip and anterior groin pain over six to nine months, along with restricted range of motion
HISTORY
A 51-year-old male patient had been experiencing progressively worsening right hip and anterior groin pain over six to nine months, along with restricted range of motion. He was constitutionally well, and underwent an initial hip radiograph for investigation.

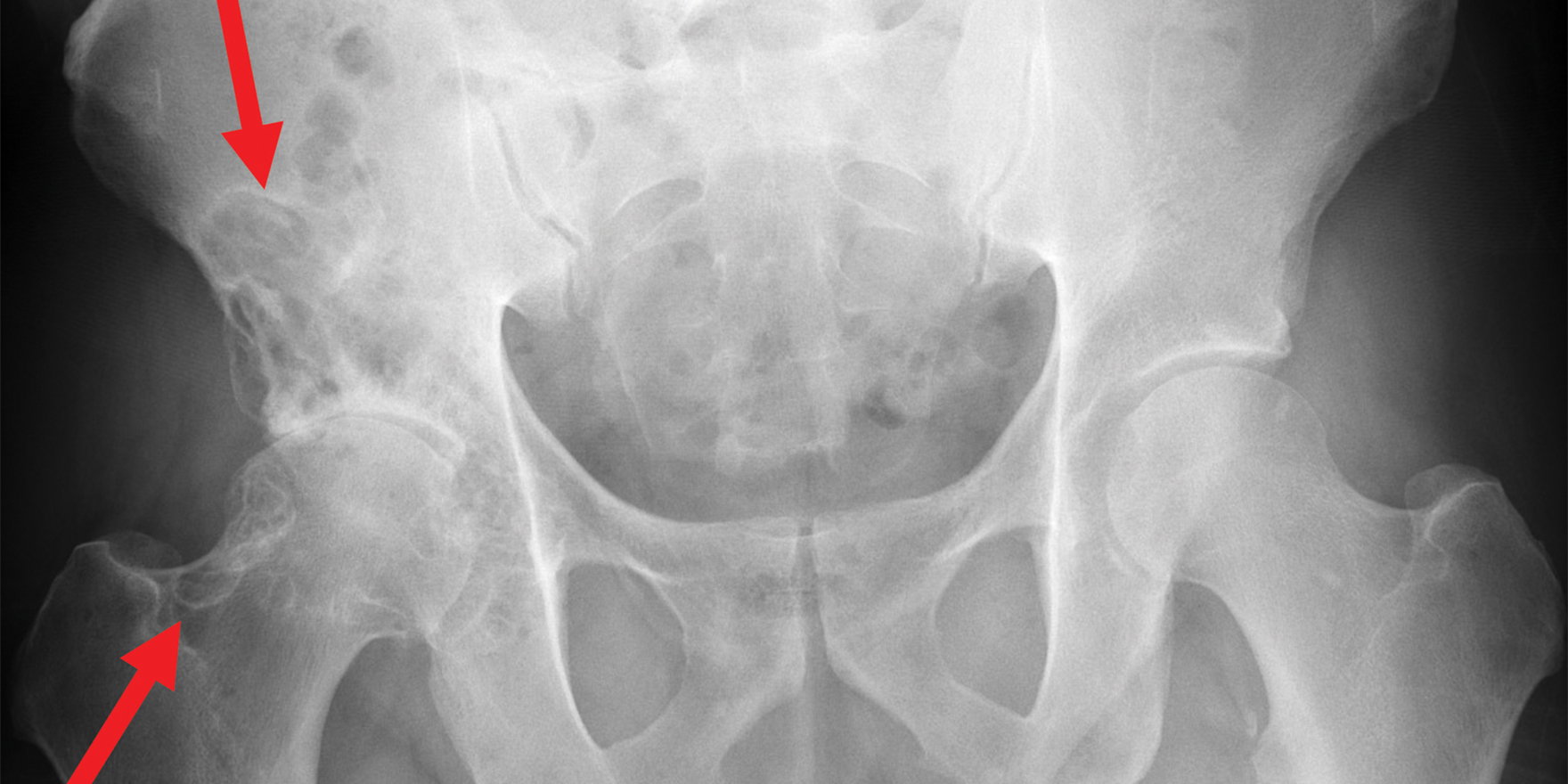
IMAGE FINDINGS
This right hip X ray (figure 1) revealed advanced osteoarthrosis with marked reduction in joint space and subchondral sclerosis. There were also prominent subchondral lucent changes which were more extensive than expected for subchondral cysts due to arthrosis on the acetabular side, extending up into the iliac wing. Additionally, subchondral and femoral neck lucencies were noted which similiarly extended beyond the usual territory of subchondral geodes due to arthrosis. These lucent changes were particularly found along the axis of the capsule.
This prompted further imaging in the form of CT and MRI.
On CT, (figures 2 a,b) there is better visualisation of the erosive bone changes, which have well circumscribed, sclerotic margins. In addition, prominent soft tissue is demonstrated within the hip joint decompressing posteriorly and inferiorly. This is non-calcified.
On MRI, (figures 3,4,5) there is correspondingly low signal to the intra-articular synovial mass-like thickening on all sequences, and only mild enhancement. Erosive bone changes and marrow oedema are well demonstrated.
DIAGNOSIS AND TREATMENT
From the radiographs and CT, one can deduce the following:
This is a joint centred pathology, as changes are seen on both sides of one joint
This is a mono-articular process (as far as we can tell)
This is a chronic process – the erosive bone changes, although striking, have sclerotic margins implying that bony remodelling is slowly progressive
There is superimposed arthrosis
With these features, the most likely differential diagnosis is that of synovial osteochondromatosis, or pigmented villonodular synovitis.
However, MRI adds the following features:
There is low signal synovial mass like thickening, which implies hemosiderin staining.
There are no cartilage bodies
Thus, diffuse erosive pigmented villonodular synovitis with secondary arthrosis is the most likely diagnosis. This was confirmed on biopsy.
Unlike in osteoarthritis, the lytic changes are not only secondary to a bone invasion of the outside of the weight-bearing area, but also due to intra-articular hyperpressure. The thick capsule that is physiologically present in the hip probably contributes to this invasion because it prevents any expansion of the joint space.
In terms of treatment, there is no well defined consensus approach to management although it is generally agreed that surgery is required. Synovectomy in non-arthritic patients, or in this case total hip arthroplasty, would be warranted.
Dr Sebastian Fung is a musculoskeletal radiologist who undertook an MRI imaging fellowship in Hospital for Special Surgery in New York. He now works in Sydney at St Vincent’s Private Hospital and Mater Hospital