The chairs of the MBS Review Taskforce strongly support the idea that GPs are not weighted correctly in the MBS in terms of overall payment
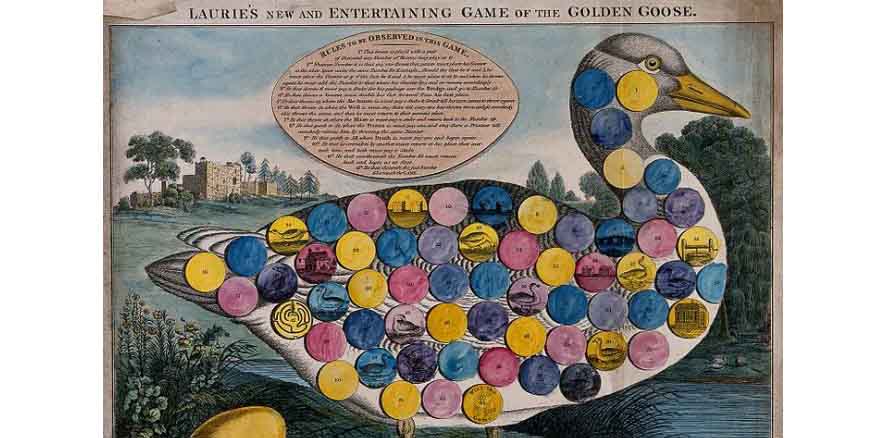
“We all know that health is the goose that keeps laying golden eggs,” is just one of quite a few horror quotes Professor Bruce Robinson, Chair of MBS Review Taskforce, has encountered while doing the review. This quote was from an investor in medical centres, referring to the profession’s ability to access government funds through the MBS.
Professor Robinson, and his taskforce deputy chair Adjunct Professor Steve Hambleton, faced a room of concerned GPs and practice owners recently to answer some of the harder questions about where the review might end up.
Professor Robinson emphasised the aim of the review was to ensure the MBS adequately and fairly remunerated high quality, evidence-based practice, not provide a menu for entrepreneurial individuals to manipulate to secure profits.
“If we keep letting people think that way then we deserve what we get.”
Under the current system, Professor Robinson estimates 5-10% of doctors are not acting in good faith. “People who are ripping off the system are going to spoil it for everyone,” he said.
He did concede, however, that misinterpretation of the MBS was not always intentional. As an example he spoke of a cardiac surgeon who always billed for a thoracotomy and chest drainage as well as the cardiac surgery, as that is what he had thought all cardiac surgeons did. These procedures are assumed, but not specifically listed, in the cardiac surgery MBS item number.
Often the descriptors for item numbers were very poor, providing opportunities for gaming the system, he said.
Professor Robinson said this first ever review, which involved more than 5700 MBS item numbers, had been much more complex than originally anticipated, taking more than twice as long as the anticipated two years.
Issues such as trying to get equity of payment for like services was often a challenge.
As an example, he described the rebate for delivering an anaesthetic for a straightforward colonoscopy which took minutes was very similar to that for giving an anaesthetic for an hours-long cancer operation. However, trying to change this situation was destined to create angst. The Australian Society of Anaesthetists called for Professor Robinson’s resignation suggesting he didn’t understand the complexities of how rebates worked for their profession and suffered from a “Robin Hood complex”.
In addition, the whole concept of applying a time-tiered payment structure across the profession has its problems. Should you reward absolute time or median or average time taken for a particular consult or procedure? How would that take efficiency and experience into consideration? A person who takes three hours to conduct a consultation or operation is not worth three times someone who can do the same thing in an hour. But, we don’t want to reward lots and lots of short consults either, Professor Robinson said.
Both Professors Robinson and Hambleton, were blunt about the situation for GPs. They were strongly in favour of the idea that GPs were not weighted correctly in the MBS in terms of overall payment.
“One of the things we recognised right from the outset which was wrong with the MBS was how general practice was being funded and paid for,” Professor Hambleton said.
It was clear that general practices were “constrained by the current funding model”, and over time it had to change in order to realise the value of GPs as the hub of an efficient system to manage the oncoming chronic care crisis, he said.
This current review is almost completed with the finalisation of the report due later this year. So far the taskforce has made 332 recommendations, with 297 of these accepted.
Some of the recommendations that affect GPs include:
- Voluntary patient enrolment at general practices
- Remuneration of GP telehealth consults
- Combining GPMP with TCAs
- Level E consult at 60 minutes or more
- Interacting more tightly with PHNs to build population data
The next phase in the review process will look at how the system can successfully move to mixed funding care models, without harming businesses and without too many “perverse outcomes”, from sending the wrong remuneration signals.
“We do somehow need to transition to blended quality care and we know what our destination looks like, but we need to be careful that we keep all these good independent businesses operating on the journey,” Professor Hambleton said.