Higher rates of high-grade precancerous cervical lesions have been detected in women hospitalised with lupus.
Higher rates of high-grade precancerous cervical lesions have been detected in women hospitalised with lupus, an Australian study has found, while no difference was detected in women with MS.
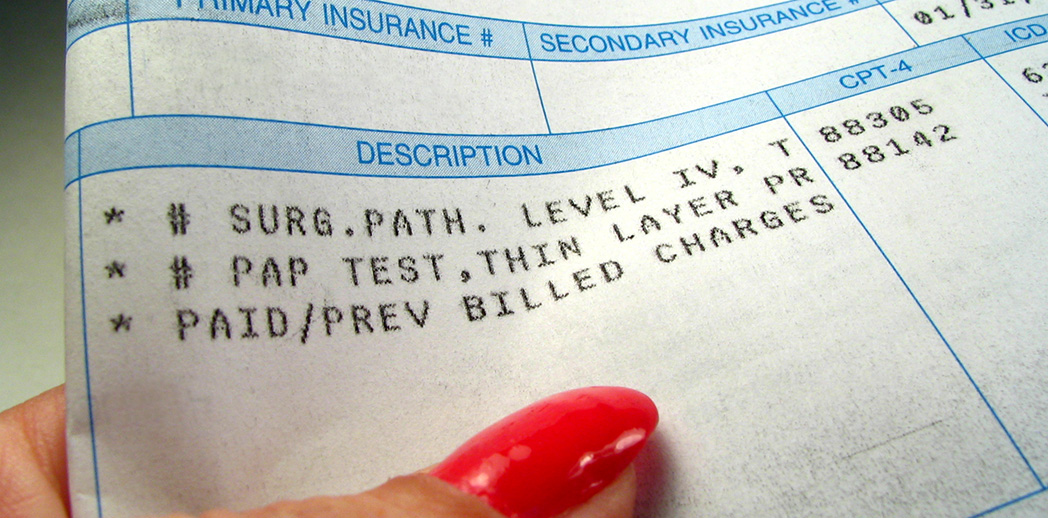
Immunocompromised individuals are susceptible to infection, including sexually transmitted infections of human papillomavirus (HPV).
Australia’s national cervical screening guidelines (which were revised in 2017) recommend that women with inherited, acquired or treatment-related immune deficiencies should be screened every three years, instead of every five years as recommended for other women.
Previous population-wide cohort studies have found that women with certain autoimmune conditions are more likely to develop precancerous cellular abnormalities on the surface of the cervix (termed cervical dysplasia), especially if treated with immunomodulatory therapies.
The first study comparing rates of low- and high-grade cervical dysplasia in Australian women with and without autoimmune disorders has now been published.
Cervical screening results were matched with public Victorian emergency department records of women hospitalised over a 14-year period with a range of autoimmune conditions, including inflammatory bowel disease, MS, RA and systemic lupus erythematosus (SLE) and/or mixed connective tissue disease (MCTD).
Of the almost 8000 women with autoimmune disorders, those with either SLE or MCTD were at most risk – around 1.5 times more likely to develop high-grade cervical abnormalities than hospitalised women without an autoimmune condition.
Rheumatologist Alberta Hoi, who leads the lupus clinic at Monash Medical Centre in Melbourne, said previous studies have reported an elevated risk of high-grade cervical dysplasia in SLE, with the use of immunosuppressant therapies, specifically azathioprine, identified as one contributing factor.
Such analyses were not possible in this study, Associated Professor Hoi said, since information on long-term medication use would not have been readily available in the hospital records used.
Moreover, many women with less severe disease might never be admitted to hospital and were therefore not included in this study.
Notably, the study was the first in the world to report rates of cervical dysplasia in women with psoriatic arthritis and enteropathic arthritis. These women had a greater risk of low-grade abnormalities than women without an autoimmune condition, as did women with RA and inflammatory bowel disease.
Dr Pierre-Antoine Dugué, an epidemiologist at Monash University who investigated cervical cancer risk in nearly 342,000 Danish women with autoimmune diseases, noted that similar to his and previous studies, several variables could not be controlled for in the Australian study.
These were “most importantly sexual history, but also other lifestyle variables that may be associated with HPV clearance like smoking or dietary habits”, he said.“There were also no available data regarding vaccination history.”
Nevertheless, Dr Dugué said this latest study was a good reminder that women with autoimmune conditions might be at increased risk of infections, including HPV-related cervical abnormalities: “It’s important that these women are reminded to participate in screening regularly.”