Secukinumab rarely reactivates latent TB, unlike some other immunomodulatory drugs, a study suggests.
TNF inhibitors and methotrexate are known for their tuberculosis risks, but the IL-17A inhibitor secukinumab is rarely associated with TB infection, a study shows.
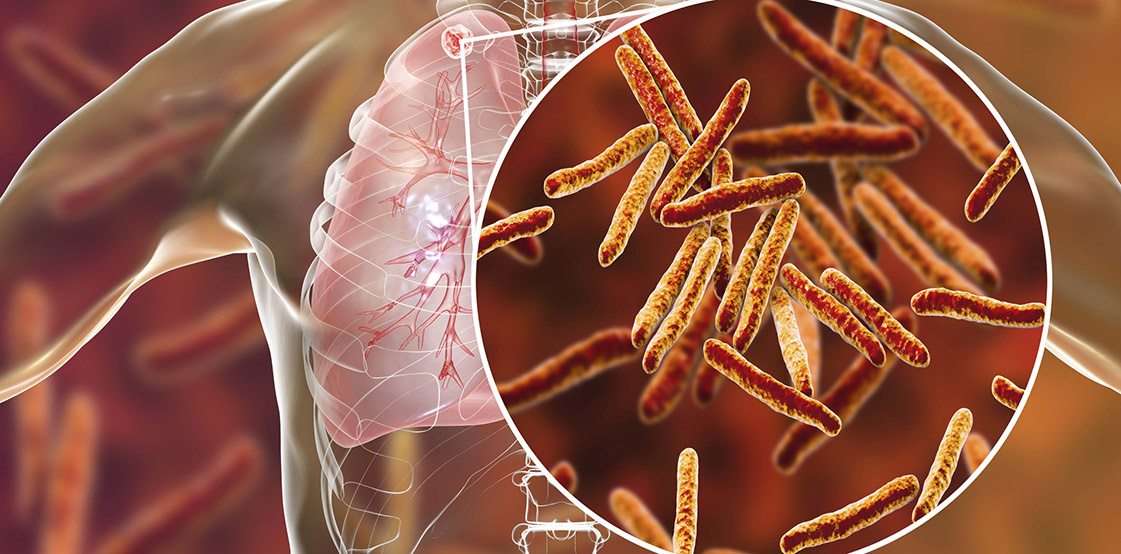
Immunosuppressant drugs have a way of coaxing dormant tuberculosis back to life, and any patient being considered for biologics usually undergoes TB screening and treatment to reduce the risks of TB infection while on these medications.
Even with diligent screening and treatment, there’s still some risk that those treatments won’t work or that patients will be newly exposed to TB in their travels overseas.
There are also some patients who cannot tolerate the TB prophylaxis, who might benefit from being put on an immunosuppressant with a lower risk of reactivating TB.
Therefore, knowing which drugs for rheumatic disease are less likely to wake sleeping TB is quite useful information for rheumatologists to have at their fingertips.
It’s been suspected that IL-17A inhibitors like secukinumab have fewer TB risks than methotrexate sodium, cyclosporine and tumour necrosis factor (TNF) inhibitors.
To examine whether secukinumab actually has a lower TB risk than other drugs, US researchers looked at data across 28 clinical trials.
These trials included more than 12,000 adults with psoriasis, psoriatic arthritis or ankylosing spondylitis who were taking the IL-17A inhibitor secukinumab.
Before being placed on this medication, the patients were screened and treated for TB and latent TB infection (LTBI).
The results, published in JAMA Dermatology in September, showed that secukinumab was very rarely associated with TB infection or reactivation of latent TB in the studies.
Over the five-year follow up period, only 13 (0.1%) of patients had a latent TB infection.
Six of these patients had a prior positive latent TB infection test result and seven were newly diagnosed.
Associate Professor Justin Denholm, the medical director of the Victorian Tuberculosis Program, said the results could be interpreted in two ways – 1) that secukinumab was unlikely to increase risk of TB reactivation by very much; or 2) that the preventative treatment worked well at stopping reactivation. “Probably, both of those things are true,” he said.
“To me, this fits with our clinical impressions that secukinumab doesn’t seem to increase risk of LTBI reactivation particularly, unlike earlier biological agents, especially the TNFa inhibitors, and to a lesser extent, oral steroids,” he said.
Blocking TNF with TNF inhibitors prevents these cytokines from recruiting immune cells to the site of the infection, which is vital for clearing TB infection. Thus, TNF inhibitors are associated with active TB and activation of latent TB infection.
“It’s reassuring to see that few people acquired LTBI while on treatment, but no systematic testing was done – so we still need longitudinal studies testing people on various biological agents over time to better understand how they influence our risk of acquiring LTBI in the first place, rather than just risk of reactivating from LTBI to active disease,” he said.
“For Australian clinicians, I’d encourage them to think about LTBI, and do a baseline assessment, for all patients.
“It’s also good to remember that some biological agents might increase the risk of acquiring LTBI, such as while travelling, and clinicians should consider whether their patients need travel advice (once we get out of the pandemic restrictions!).”
While TB infection is rare in Australia, around 5% of Australians (and around 17% of Australians born overseas) have latent TB.
It’s uncommon for latent TB to reactivate; it only happens in about one in ten cases. But reactivation becomes more likely if a person is taking immunosuppressants.
Associate Professor Paul Bird, a rheumatologist based in Sydney, said this was “an interesting study with large numbers”.
The results should be a message on continuing to screen all patients for TB using the QuantiFERON-TB blood test and a chest x-ray, rather than an endorsement of secukinumab as a low-risk agent, he said.
“Screen for TB before biologics, AND screen patients after travel to at risk areas OR if there has been a suspected exposure,” he said. “These are the main take away messages.”